Change Makers: Dr Valerie Montgomery Rice on Healthcare Disparities and Moving from Talk to Action
Dr. Montgomery Rice speaks with Dr. John Whyte about the need for an increased proportion
of
healthcare providers of color and strategies for building healthcare equity for all.
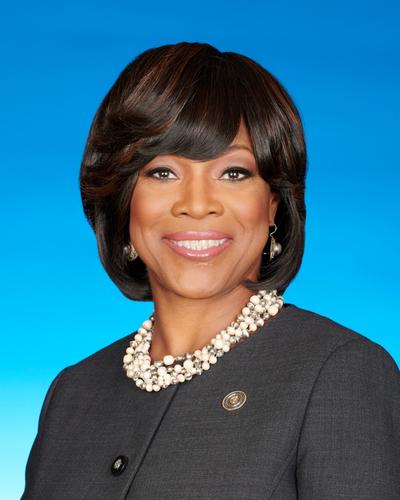 Dr. Valerie Montgomery Rice
Dr. Valerie Montgomery Rice
President & CEO, Morehouse School of Medicine
By Dr. John Whyte, Medscape
This transcript has been edited for clarity.
John Whyte, MD, MPH: I'm Dr. John Whyte, the chief medical officer of WebMD. We've spent a lot of time over the past 2 years addressing ways we can fight healthcare disparities. One strategy is to increase the number of minority physicians, nurses, and pharmacists. But that doesn't happen overnight. My guest, Dr. Valerie Montgomery Rice, President and CEO of Morehouse School of Medicine, tells us why we need cultural humility, as well as a greater emphasis on genomics and personalized medicine, if we truly want to overcome disparities. She talks about why she's a "glass-half-full" instead of "glass-half-empty" type of person. And she explains why she doesn't get angry over the low number of physicians of color in specialties like orthopedics and cardiovascular surgery. Rather, she's hopeful about the future. But we also chat about the past, where she tells us about her own journey in medicine. You might be surprised by her answer as to whether it was harder to be a woman or a person of color.
Dr. Montgomery Rice, thanks for joining me today.
Valerie Montgomery Rice, MD: It is my pleasure, Dr. Whyte, to be with you.
Whyte: You and I have talked about disparities for years. I want to start off with, how has the COVID pandemic addressed disparities? Is it simply raising awareness or are we actually going to do something differently now?
Montgomery Rice: You know, John, what COVID-19 did for us was raise awareness. But more importantly, it raised awareness for people who perhaps had had blinders on for long periods of time. We've known that health disparities existed based on race, ethnicity, gender, socioeconomic status. And what the COVID-19 pandemic showed us was that even when you could afford medications, you didn't necessarily have access to them. So, access to the vaccines, but even before that, access to testing. And even more importantly, what we were able to see were the differences between the "haves" and the "have-nots," really based on socioeconomic status more so than race.
Whyte: But do you feel that it's finally going to be addressed? As I've referenced, you and I literally have talked about this for about 15 years. So do you feel now that there's a commitment? Or is it going to be something in a year or two, where if people aren't paying attention to it, we're not going to address it? How do we sustain this interest and in truly addressing disparities?
Montgomery Rice: I'm hopeful, but I'm also… As you said, we've been doing this for a long time, right? What I also believe happened differently with this pandemic than what we've seen before is that it was so much in people's faces — the injustices that lead to health disparities, that lead to poor health outcomes. And many people for the first time began to see the root of the problem and started to say, "Okay, it's not just that African Americans or Latinx people have more diabetes or hypertension; there are some things that led to that." Perhaps they live in food deserts, perhaps they don't have access to providers at the same rate as majority persons, or perhaps they don't have access to all the medications or opportunities for preventive health. And I think people really began to see the social injustices that lead to health disparities that lead to poor health outcomes. Now, what we fortunately saw was that many of those injustices were talked about in people's living rooms, on TV, in webinars and seminars, among people who have not had those previous conversations. That is what gives me hope.
Whyte: But we have to move from talk to action. And one of the solutions that people have suggested is that we need more people of color in the healthcare workforce. We need more doctors, nurses, pharmacists. Here we are at Morehouse School of Medicine, with the president and CEO. You're an educator running an institute of higher learning. But let's go back to the pandemic. The pandemic — and you've been very vocal on this — has disproportionally impacted historically Black colleges and universities, institutions like Morehouse School of Medicine. So help explain to our audience: Why has the impact been different here on students than perhaps at some other institutions?
Montgomery Rice: Let me unpack this question because it does have some historical context. I'm going to take you back to many, many years ago when I was at Meharry Medical College and we first met. You were at Discovery Channel, and we were looking at a lack of diversity in the public health workforce. And you and I worked together to raise awareness to students of color at historically Black colleges and universities (HBCUs) about a public health degree and the opportunities for that. We thought that that would help with preventive healthcare and raising awareness around population health issues around diseases. And we had a lot of success with that.
I look at that as something that was very important but not necessarily a continuum. We see the same thing that has happened, as we're educating and training providers or healthcare professionals — MDs, nurse clinicians, etc. — that people are doing spotty work with trying to increase the diversity in the classroom, but they need to understand that it can't just be on the backs of the HBCU medical schools. We need all of the medical schools — all 150-plus — to be committed to diversification of the healthcare workforce. And why is that? Because the data have shown that when you have race concordance, gender concordance, and cultural concordance between the provider and the patient, you have improved outcomes, and those improved outcomes come about because of trust and people being willing to take the advice of their provider and adhere to the recommendations. And it also leads to the opportunity for providers to learn from their patients how to co-create new solutions that align with meeting the patient where they are. And so that cultural competence also includes cultural humility, the ability to be willing to learn from someone who you are trying to provide benefit to. I think the COVID-19 pandemic showed us that we really do need this, this diversity of the healthcare workforce, if we are going to change the hearts and minds of individuals that we're trying to care for.
Whyte: I want to push you a little more on this issue of people of color in the health professions because we just can't turn the spigot on, like we've talked about, and have them come out. Over your time here at Morehouse School of Medicine, you've increased enrollment significantly, but as you said, it can't just be one person in one institution. I want to read you some statistics: The most recent percentage of Black men among medical school graduates has been 7% — 7%!
Montgomery Rice: For the past 15 years.
Whyte: Yes. Now it's slightly improved, partly because of some of the efforts that you've talked about in terms of matriculants (those people that have enrolled) — 11%. But there's something that people aren't talking enough about that I want to hear your thoughts on. If we look at the number of people of color, particularly Black men, in surgical specialties — let's take orthopedics — to find a man of color as an orthopedic surgeon is a rare bird.
Montgomery Rice: It's rare.
Whyte: Does it make you mad?
Montgomery Rice: No, it doesn't make me mad; it makes me anxious to do more. If you look at any of the surgical specialties or inpatient opportunities in ER or anesthesiology, it's less than 5% people of color — less than 5%, for sure, African American. And that is because, John, there is clear bias in how we select residents, people who finish medical school and go into residency training. Now, have we tried to put forth efforts to eliminate some of that bias? Yes. And one of the things that we started 2 years ago was to make USMLE Step 1 pass/fail, because many people had used that as the gateway to determine whether or not people could go into some of the surgical specialties. That's no different than what we see with the MCAT and GPA for people getting into medical school.
One of the great things that we do at Morehouse School of Medicine is shift the curve; we get on average 7500-9000 applications a year for 125 slots. So, John, if we chose to, we could select everybody with a 4.0 GPA and MCAT scores in the 90th or 95th percentile, but that may not align with our mission or our vision of leading the creation and advancement of health equity. So, what do we do? We take academically diverse students. Many of those students are first-generation college students, many of those students may come from challenging households, many of those students may come from underserved rural communities. We take those students and within 2 years we can shift the curve. And what do I mean by that? When you look at their Step 1 pass rates or scores compared with other students who came in with these high GPAs and came from these affluent families, they are doing just as well.
Whyte: Alright. Well, let's talk about success. And let's use Dr. Valerie Montgomery Rice as our example. Here you are, a woman of color, went to Harvard Medical School — not many women of color, and there were not many people of color in general at the time that you went — became an expert in infertility. Again, not the typical field where you see lots of people of color. Since I've known you for a long time, I want to brag for you: Your portrait hung in the National Portrait Gallery as part of The Black List of successful people of color. Why have you succeeded?
Montgomery Rice: I have succeeded because I have always had a strong support system, which started with my mother, who was a single parent of four girls, who left my father from an abusive relationship because she wanted something different for her girls. But also because we had a network of church members and others who supported us. And throughout my career, I have had mentors and sponsors who saw something in me that I sometimes didn't see in myself, and they helped create an opportunity for me to be successful. Now, the other thing is that Valerie Montgomery Rice works hard. Hard work has never bothered me; it is something that I believe is necessary in order to become an expert. The third thing is that I've always been open to listening to others, to gain insight on what's possible. And if you can humble yourself enough to be able to ask a question when you're sitting across from somebody, you're going to be amazed at the information that they will share once they become comfortable that you are aligned in seeking an opportunity to learn from them. And it also then leads to greater success for you.
Whyte: But even with all that, let's put it in perspective. You broke down a lot of institutional barriers; even with that support system, you still had to overcome a great deal. And here you are, leading a prestigious institution of higher learning. What's Dr Montgomery Rice's leadership style? How did you break down those barriers? And you continue to do so.
Montgomery Rice: Clearly, my leadership style has changed as I have matured — how about that?
Whyte: I have known you a long time, so I would agree with that. What can people learn from you?
Montgomery Rice: What I have always tried to do, John, is to be in the moment and to understand my environment. And again, understand that teamwork is what will lead to greater success. I've always tried to surround myself with diverse thinkers. I always talk about cognitive diversity: I think about the life experiences that people have had, because I think that that is going to help them have a different outlook on how we solve for a problem, and the richness of the solution is going to be greater because of that. So, I think my style is collaborative. I am aggressive, in the sense that I like to see change occur. But no one wants to be successful by themselves, so I've learned over the years that a collaborative spirit in inviting other people to bring their ideas to the table creates ownership, and then we all get to share in the success. The other thing that I have learned in my leadership growth is to be more empathetic toward others, to really understand that people do come sometimes with baggage that is not visible, and you need to extend grace sometimes for them to unload that baggage, in order to pick up some of those new skills that lead them to their growth.
Whyte: Do you have to think about it differently? As a woman? As a minority? Does that ever factor into your mind?
Montgomery Rice: You know, John, that's an interesting question. People have always asked me what was harder: being a woman or being African American or Black. And I would say being a woman — I felt most invisible in rooms where there were only men. I rarely felt invisible because I was a Black person. It was more so because I was the only woman and because of, like you said, the field that I chose — reproductive endocrinology— early on.
Whyte: Surprisingly not a lot of women.
Montgomery Rice: Not that many women, right? Even though OB/GYN has a lot of them, but not reproductive endocrinology. But my mentor, the person who inspired me to be a reproductive endocrinologist, was Dr Isaac Schiff, a Caucasian man and leader at Harvard Medical School. It was his bedside manner of how he treated his patients, along with the opportunity to make a difference in couples' lives — to be able to have children — that really inspired me to do reproductive endocrinology.
Whyte: This series is also about change makers. You've pointed out how you've been a change maker. I also want to go back to that concept of health and how we're thinking differently about what health means — less so about what happens in the doctor's office as opposed to what happens at home and social determinants. How do you think our concept of health is changing?
Montgomery Rice: One of the things that we have done at Morehouse School of Medicine is to really take a deep dive into looking at health disparities and trying to look at it with a glass-half-full approach in talking about health equity. We define health equity as giving people what they need, when they need it, and the amount they need to reach their optimal level of health. And when we think about what that person needs, it can be different for even "affluent" people. You may have juvenile diabetes and you may need the next therapy in order to reach your optimal level of health. You may have cardiovascular disease and you may need that next surgical intervention to reach your optimal level of health. And that's what we mean about giving people what they need, when they need it, and the amount that they need. And then for some people, it's the social determinants: access to a doctor, transportation to a doctor, having advanced cancer and having access to a clinical trial. Those are the things that we have to think about when we look at individuals and understand what they need, because health is defined differently depending on where the individual is. At Morehouse School of Medicine, one of our vision imperatives is building a bridge between healthcare and health. What is it that needs to be on that bridge so I can walk across it?
Whyte: What needs to be on it?
Montgomery Rice: Right — what needs to be on it? It depends on where I am found at the beginning of my healthcare journey. It depends on what disease is impacting me. Or if I'm a young, healthy individual already, again, those screening tests. Let's talk about access to vaccines and getting over the vaccine hesitancy. We had to put education and trust on that bridge so that African Americans and Latinx persons would be able to receive that healthcare to be able to walk across that bridge to health.
Whyte: Take out your crystal ball. What does the future of health look like 5 years from now?
Montgomery Rice: I believe that the future of health is going to have to continue to address the social determinants. We need to eliminate the barriers of access to care. Everybody ought to be able to have what we believe are the basic opportunities for access to care: screenings, annual exams, annual mammograms, colonoscopies at the right time, access to vaccines, etc. And then we need to move along a continuum of what I call precision medicine. So we need to think about the value proposition of genomics, which allows you to look at me more as an individual and be able to prescribe medications to me based on how I am going to respond to the individual medications that are out there. I believe that genomics and precision medicine will be very, very important as we move along this continuum of building this bridge between healthcare and health. Now, when you talk about people of color, we are once again going to have to create an educational opportunity, such that people see the value proposition of why they need to be a part of building this enhanced database of genomics. You know, the genome was constructed with only about 2.4% of African American, and so that is not reflective of the diversity that we believe exists, and it may end up hindering our ability to be as precise with precision medicine if we don't have a database that reflects the general population.
Whyte: Dr Rice, I want to thank you for taking the time today to sit down and chat, and to share what you see are the insights we gained from COVID, as well as what the future may hold for health. Thank you.
Montgomery Rice: You're welcome. Thank you for having me.

