Eight Prominent Black Leaders in Medicine
MSM President and CEO Dr. Valerie Montgomery Rice and former MSM President and US Surgeon General Dr. David Satcher are among the leaders featured by AAMC.
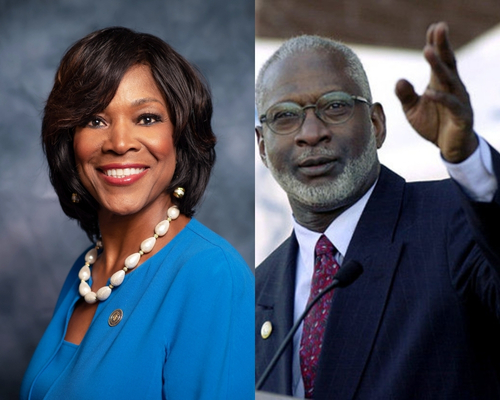 (L-R) Dr. Valerie Montgomery Rice, President & CEO, MSM and Dr. David Satcher, former
MSM President and US Surgeon General
(L-R) Dr. Valerie Montgomery Rice, President & CEO, MSM and Dr. David Satcher, former
MSM President and US Surgeon General
By Stacy Weiner, AAMC News
They have created campaigns to battle opioid addiction, re-envisioned violence prevention, and discovered a breakthrough treatment for sickle cell disease. They have run medical schools, chaired the nation’s first health equity task force, and served as the first African American to lead the Centers for Disease Control and Prevention (CDC). Often, their success came despite poverty, racism, and great personal loss. In honor of Black History Month, we share the incredible stories of eight contemporary medical leaders.
Valerie Montgomery Rice, MD, FACOG
Valerie Montgomery Rice, MD, FACOG, was raised in a chaotic household. Her father abused her mother, and even burst through the window of their Macon, Georgia, home one night with a gun.
Her school life was also difficult. In second grade, a racist teacher told her that she need not bother trying to learn.
But Montgomery Rice’s mother told her, “All things are possible. There are no limitations.”
Today, as President and CEO of Morehouse School of Medicine (MSM) — the first woman in that role — Montgomery Rice works to convey that message to scores of future physicians.
Since taking the helm at MSM in 2014, Montgomery Rice has nearly doubled the number of MD candidates and enhanced its research labs. In 2022, MSM joined the newly launched Accelerate Precision Health partnership, part of the Chan Zuckerberg Initiative, to advance precision medicine for everyone, particularly people of color.
The Harvard-trained OB/GYN is also a world-renowned researcher, and she has been particularly dedicated to exploring infertility and addressing maternal mortality rates among Black women. At Meharry Medical College in Nashville, where she served as dean before moving to MSM, Montgomery Rice founded and directed one of the first centers focused solely on studying conditions that disproportionately impact women of color.
Reflecting on her MSM role, Montgomery Rice has said, “Medicine allowed me to find my passion, and leadership allowed me to find my purpose…. I didn't even know something like this existed for people like me. So I have come to a place that I didn’t expect, but I know I’m in the right place at the right time.”
Griffin Rodgers, MD
Griffin Rodgers, MD, knew from a young age that he wanted to care for patients, particularly those in underserved communities.
After all, Rodgers — who now directs the National Institute on Diabetes, Digestive, and Kidney Diseases (NIDDK) — deeply admired his mother’s work as a New Orleans public health nurse in the 1960s.
But when Rodgers lost three close friends to the painful blood disorder sickle cell disease (SCD) during high school and college, he knew he also wanted to pursue biomedical research.
Rodgers went on to receive his medical degree from Brown University in 1979, and after completing a residency in internal medicine and a fellowship in hematology, began conducting research at NIDDK, part of the National Institutes of Health outside the nation’s capital.
In 1998, the Food and Drug Administration (FDA) approved the first-ever medication to treat SCD, hydroxyurea, thanks to Rodgers’ research.
Previously, doctors had little to offer SCD patients — which affects millions of people of African descent — other than blood transfusions. By sparking the production of healthy blood cells, hydroxyurea significantly reduces pain, hospital stays, and other SCD problems. It can even increase life expectancy of patients.
Today, Rodgers continues to research blood disorders. But as NIDDK director, he is also responsible for nearly 700 employees working to address some of the country’s most common, costly, and chronic diseases.
Rodgers has spent practically his entire career at NIDDK, rising to director in 2007. In that role, he oversees wide-ranging efforts, from work on an artificial pancreas to the creation of the most comprehensive atlas of the human kidney.
In 2023, the Institute released Pathways to Health for All, a multistep research effort to address health inequities in the United States, including the reality that African Americans are four times more likely to develop kidney failure than White people.
Of leading the Institute, Rodgers expresses gratitude for being able to accomplish even more than what he could achieve through his own research. “Being an administrator … you can make a lasting contribution potentially to millions, perhaps hundreds of millions, of people worldwide,” he has said.
Deborah Prothrow-Stith, MD
For decades, violence in America was seen simply as a matter of crime and punishment. But Deborah Prothrow-Stith, MD, believed violence was a public health problem.
Prothrow-Stith — now dean of the Charles R. Drew University College of Medicine and Science in Los Angeles — came to that conclusion during her residency in a Boston emergency department (ED) in the early 1980s. After a stabbing victim declared he would soon avenge his attack, she recognized that EDs were too often practicing revolving-door medicine.
So Prothrow-Stith threw herself into researching violence, ultimately concluding that it needed an approach much like that used in addressing HIV/AIDS and smoking: through education and prevention. In 1991, she released Deadly Consequences, the first book on youth violence for a mass audience. Prothrow-Stith also created groundbreaking conflict-resolution curricula for children and teens that were ultimately adopted in schools across all 50 US states.
But Prothrow-Stith was not satisfied with researching and writing alone.
Over her career, her leadership contributions have included serving as associate dean of the Harvard T.H. Chan School of Public Health. In 1987, she became the first woman, first Black person, and youngest individual to serve as Massachusetts Commissioner of Public Health. There, she expanded treatment for HIV/AIDS and substance use disorders and created the first Office of Violence Prevention in a state department of public health.
Last year, Prothrow-Stith was involved in another first: the establishment of an independent medical school at Drew University, the only historically Black university west of the Mississippi. Until then, the school graduated physicians through a partnership with the University of California Los Angeles.
Prothrow-Stith notes that the school will work to attract trainees from South Los Angeles, a severely underserved region, through such efforts as mentoring students as early as kindergarten.
“There’s nothing like training people from the communities that they’re going to serve because that’s where it gets authentic,” Prothrow-Stith told The Guardian last year. “That’s where the level of empathy and the appreciation of humanness comes in. It’s what medicine has needed.”
Marcella Nunez-Smith, MD, MHS
At the height of the pandemic, when President Biden needed someone to spearhead his COVID-19 Equity Task Force, he turned to Marcella Nunez-Smith, MD, MHS. In January 2021, the Yale researcher and educator became the first-ever presidential advisor to focus solely on combating race-related health inequities.
Nunez-Smith had already spent months helping shape the incoming administration’s pandemic strategy as co-chair of President-elect Biden’s COVID-19 Advisory Board, but the new role represented a decades-long passion.
As a young girl growing up in the US Virgin Islands, Nunez-Smith saw her father suffer a debilitating stroke, the result of the territory’s inequitable health care. She vowed that no other family should face a similar fate.
Today, Nunez-Smith continues to pursue that aim with a wide-ranging portfolio.
She directs the Yale Equity Research and Innovation Center, which she founded in 2013, and a two-year health equity leadership program at the Yale School of Management. Her own research includes a project to develop a questionnaire that effectively measures patients’ experiences with discrimination in health care.
Motivated in part by personal brushes with racism — patients have assumed she’s come to empty their trash — Nunez-Smith has also published widely on the experiences of underrepresented individuals in medicine.
Looking ahead, Nunez-Smith hopes the United States will no longer tolerate the deep inequities that COVID-19 exposed.
“I imagine a future for our children and their peers, where they look back at this time with historical interest [and say]: ‘Oh my goodness, can you believe the pandemic ravaged communities differently? That would never happen now!’” she has said. “That's what I want them to inherit.”
Alister Martin, MD, MPP
A fundamental vision drives Alister Martin, MD, MPP: Doctors should aspire to treat not only patients’ bodies but also the broader body politic.
Martin — an emergency medicine physician, Harvard Medical School assistant professor, Harvard Kennedy School researcher, and advisor to the US Department of Health and Human Services — has pursued that goal in multiple domains.
His first effort focused on the millions of Americans struggling with opioid use disorder (OUD).
In 2017, Martin founded Get Waivered to help physicians obtain the then-required Drug Enforcement Agency waiver to prescribe buprenorphine, an effective OUD treatment. Previously, most EDs sent opioid users home with little more than the names of detox programs.
In 2019, he took aim at patients’ lack of access to voting — something he viewed as a social determinant of health — by creating the nonpartisan Vot-ER. The initiative has drawn more than 26,000 U.S. health care providers to such efforts as helping patients obtain emergency absentee ballots so they can vote right from their hospital beds.
During the COVID-19 pandemic, he co-founded an organization called GOTVax, which used a get-out-the-vote framework to bring vaccines to under-resourced communities in Boston. Not long after, he was named a White House fellow for 2021-2022.
Among Martin’s most recent projects is Link Health, an outreach program that addresses the digital divide by helping low-income patients gain Internet access for telehealth.
Growing up the son of a single mother in New Jersey, Martin knew the toll of uneven access to health care. He also saw the power of the ED to help address it.
EDs “are not just about taking care of gunshot wounds and stroke,” but can also help lower-income individuals tackle key health inequities, he has said. “We have a responsibility, I believe, to try to address those issues for the people who have no other options.”
Selwyn M. Vickers, MD
Growing up in Alabama during the Jim Crow 1960s, Selwyn M. Vickers, MD, could not have envisioned a future as a world-renowned cancer surgeon and researcher.
But he did have powerful mentors to inspire him.
His maternal grandmother traveled 120 miles to attend high school, and his grandfather chose to learn to read and write in his 40s. His uncle, a successful doctor, sparked a similar dream in the young Vickers.
Today, Vickers impacts the care of thousands of patients each year as president and CEO of the Memorial Sloan Kettering (MSK) Cancer Center in Manhattan.
By the time he became the first African American to head MSK in 2022, Vickers had already filled numerous other leadership roles, from president of the American Surgical Association to dean of the UAB Heersink School of Medicine in Birmingham, Alabama.
In every position he holds, health equity is a guiding goal.
He pursues this aim both in clinical care and academic research and helped to establish such efforts as Enhancing Minority Participation in Clinical Trials (EMPaCT), a network that works to diversify biomedical studies, and the Center for Healthy African American Men, a first-ever academic-community collaboration to develop, implement, and evaluate interventions designed to improve African American men’s health.
“What drove me was the legacy of the challenge that this country has been dealing with since [abolition in] 1865,” Vickers has said. “[The United States] continually created second-class citizenry for people of color. That’s been pervasive in several areas,” he added, “economics, education, and certainly not the least of them, health care.”
David Satcher, MD, PhD
David Satcher, MD, PhD, knows personally the dangers of medical racism. At age two, barely able to breathe from whooping cough, Satcher was barred by Alabama’s segregationist rules from receiving care at any nearby hospital.
Thanks to the area’s only local Black doctor, who tended to him on his parents’ farm, Satcher managed to survive.
Motivated by that experience, Satcher went on to pursue family medicine — and subsequently to serve in positions of groundbreaking national leadership.
After earning MD and PhD degrees from Case Western Reserve University in Cleveland in 1970, Satcher held administrative and teaching positions at both the UCLA School of Medicine and School of Public Health. From 1982 to 1993, he served as president of Meharry Medical College in Nashville.
In 1993, Satcher became the first African American to direct the CDC. In 1998, he was appointed US Surgeon General. In that role, he focused on such crucial issues as tobacco use among minority groups and the need for school-based sex education to prevent disease and unplanned pregnancy.
After leaving government service, he founded the Satcher Health Leadership Institute (SHLI) at Morehouse School of Medicine in Atlanta with the aim of addressing health disparities through research and leadership training. Satcher’s own research revealed a disturbing reality: more than 886,000 deaths could have been prevented from 1991 to 2000 if African Americans had received the same care as white people.
Stepping up to lead, as well as training others to lead, has always been important to Satcher — he spearheaded civil rights sit-ins as a college student and facilitated President Clinton’s apology for the notorious Tuskegee experiments in 1997.
Among his advice to others is recognizing that leadership sometimes requires personal sacrifice. “That’s how it was with going to jail as a student hoping one day to go to medical school,” he has said. “It was a risk [but I knew that] if I was going to be a leader, I had to stand for something.”
James Hildreth Sr., MD, PhD
When he was a young boy, James Hildreth, MD, PhD, suffered two tragedies: the death of his father from poorly treated cancer and the assassination of Martin Luther King, Jr.
The losses were so devastating that Hildreth — now president and CEO of Meharry Medical College in Nashville — barely spoke to anyone for months. But then he decided to channel his pain into something positive by becoming a doctor.
Hildreth not only went on to achieve that goal but has since served as a leader in the battle against two devastating diseases, HIV/AIDS and COVID-19.
In 2021, President Biden appointed Hildreth to his Health Equity Task Force, where the Rhodes Scholar helped craft recommendations for addressing the pandemic’s inequitable burdens. Hildreth also helped assess the groundbreaking COVID-19 vaccines when they were submitted for FDA approval.
Hildreth was accustomed to leading: He had already served as dean of the UC Davis College of Biological Sciences and associate dean at the Johns Hopkins School of Medicine.
Also a world-renowned researcher on HIV/AIDS, Hildreth has contributed to that field with more than 100 peer-reviewed publications, 11 patents, and the discovery of pivotal aspects of the virus’s deadly power.
Since taking the helm at Meharry in 2015, Hildreth has helped the nation’s largest private historically Black academic health sciences center achieve national recognition by establishing the first US school of global health. Expected to open in 2026, the institution will promote creative collaborations among emerging health leaders around the world.
Under Hildreth’s leadership, Meharry made another bold move in 2023: It launched a 10-year initiative to create the first genomics database of people of African ancestry. Working together with major pharmaceutical companies, Meharry intends to collect genomic data from up to 500,000 volunteers. The goal is more equitable medical research and better treatments for Black populations worldwide.
“Starting today … we begin to leave the past in the past where it belongs,” Hildreth said in announcing the initiative. “[It] will ensure that — at last — our future, and the future of generations to come, will be different from those who came before.”

