Digital Technology Study
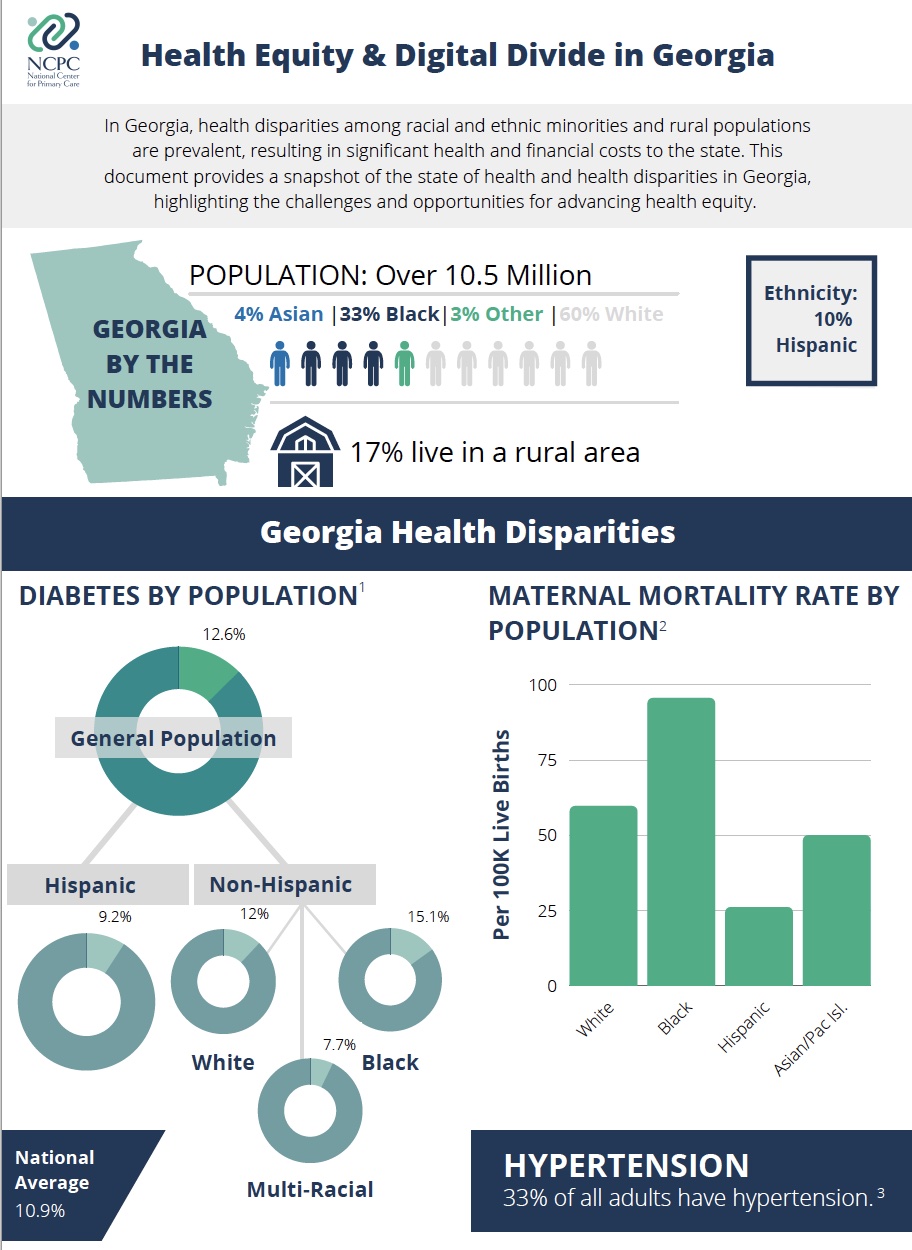
Despite tremendous potential for technology to aid in the advancement of health equity, our prior research1 has identified gaps in technology adoption that impact high disparity populations.
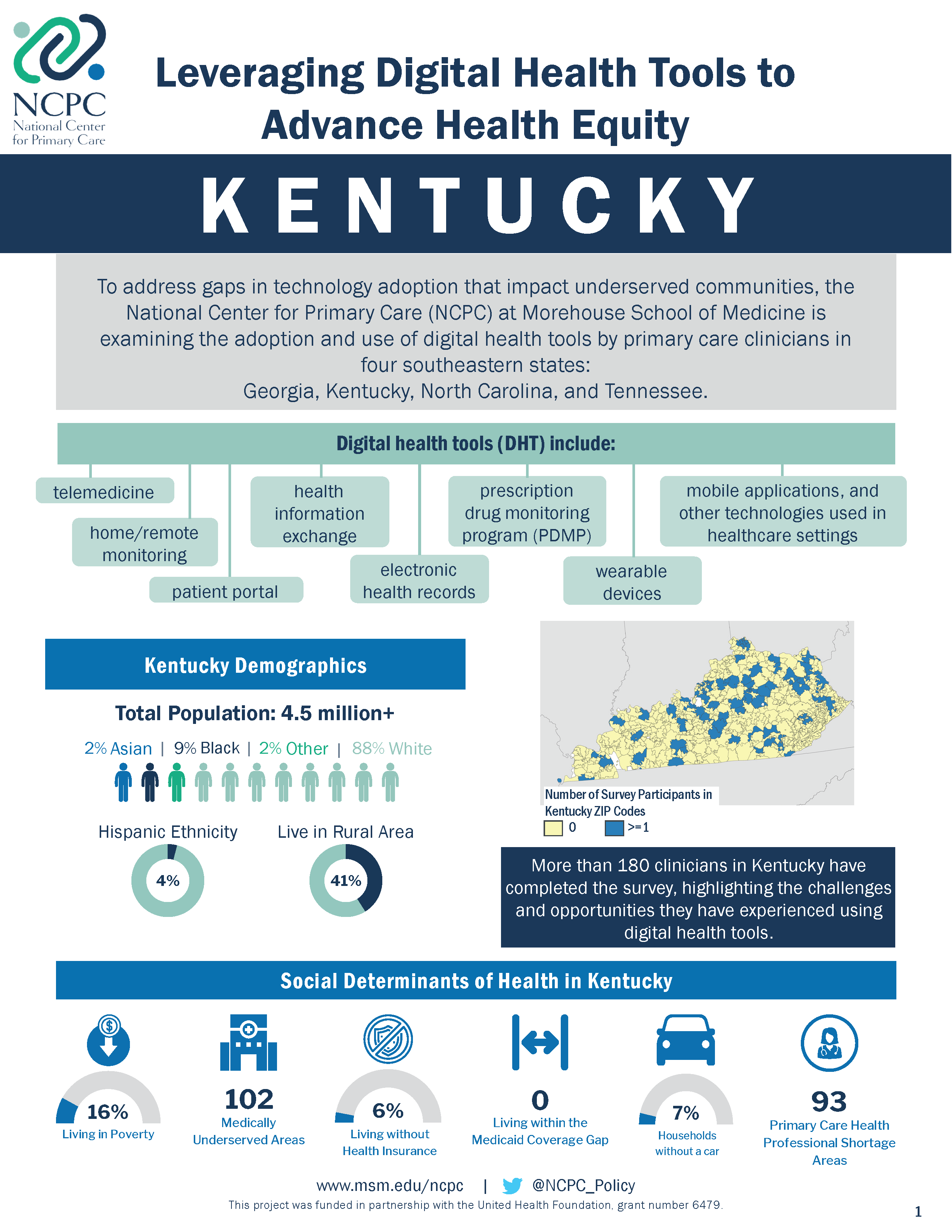
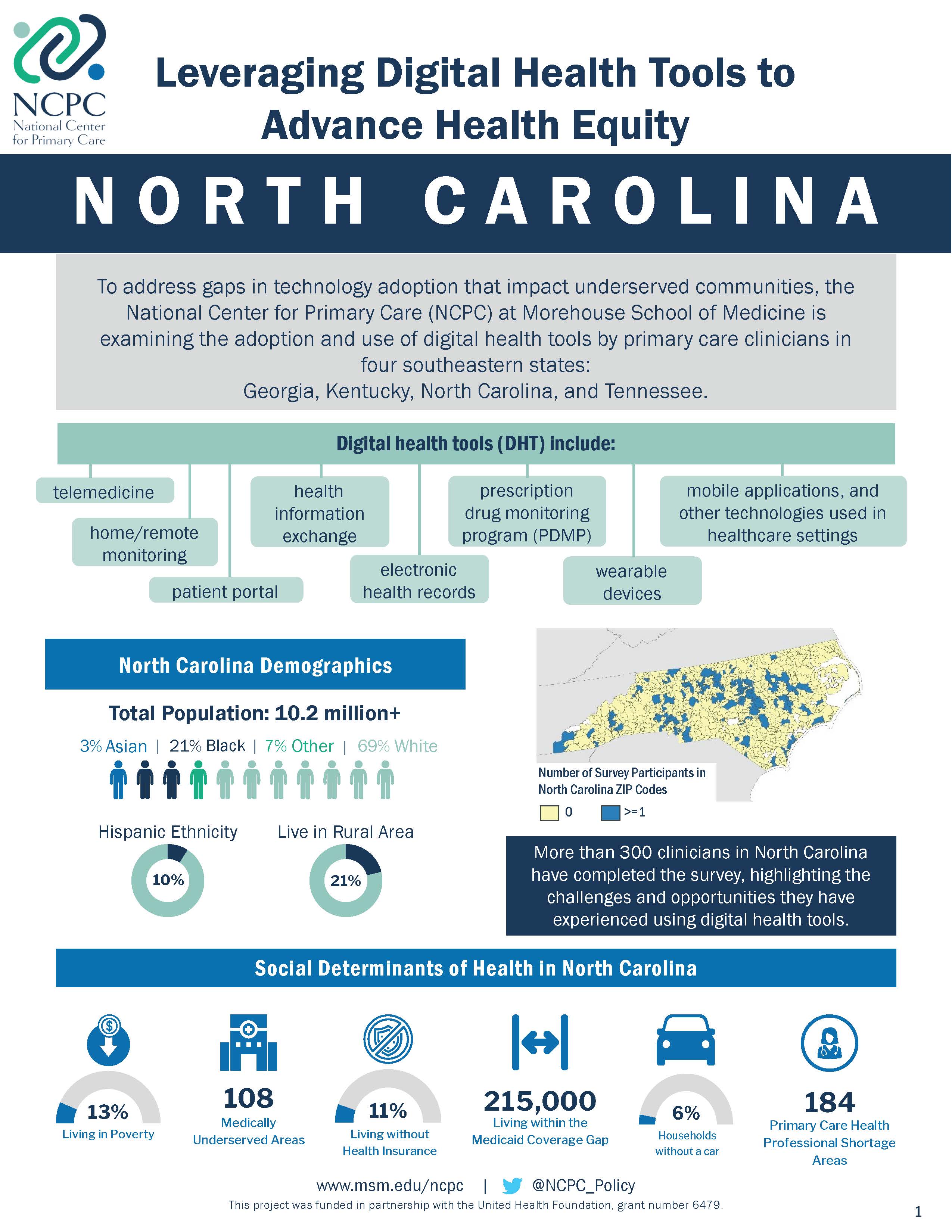
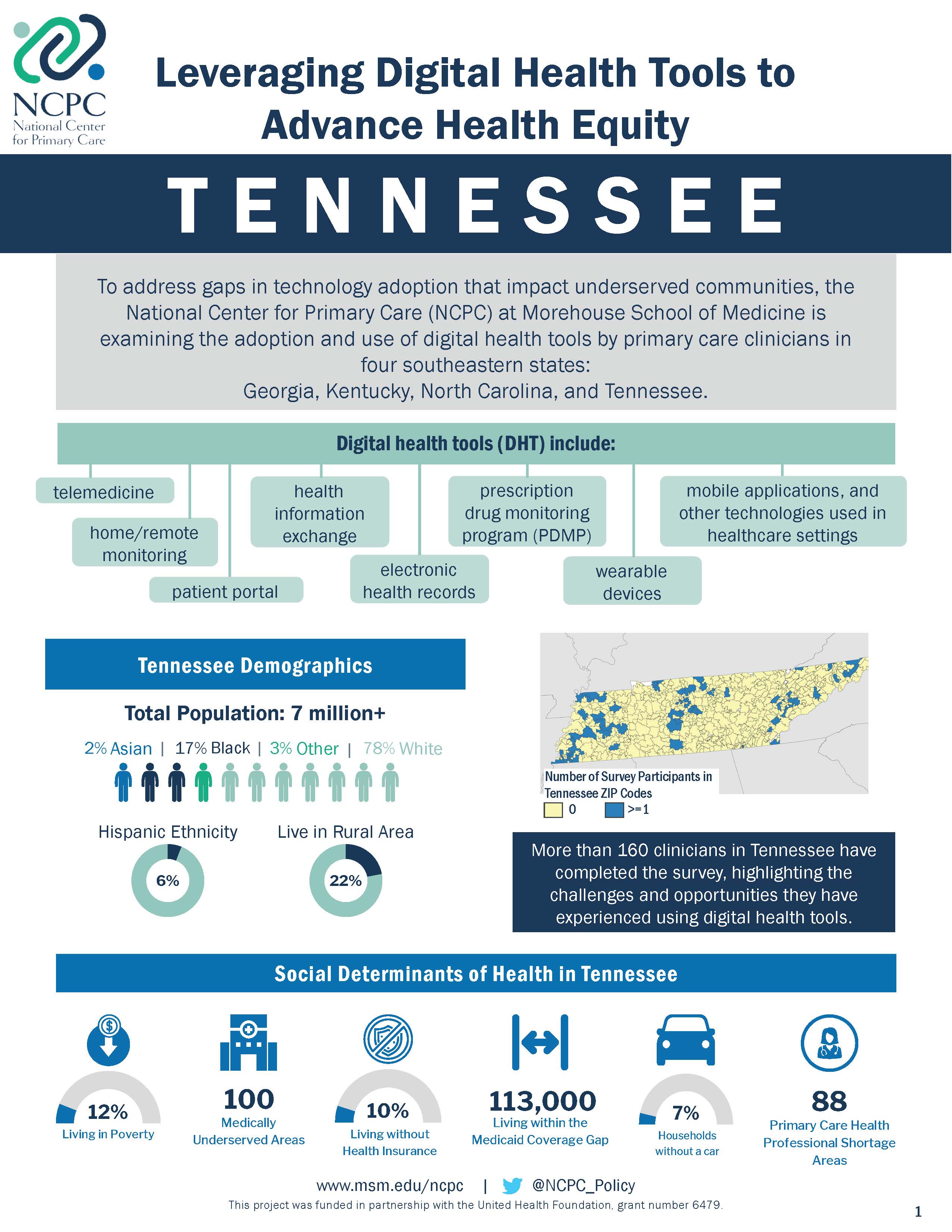
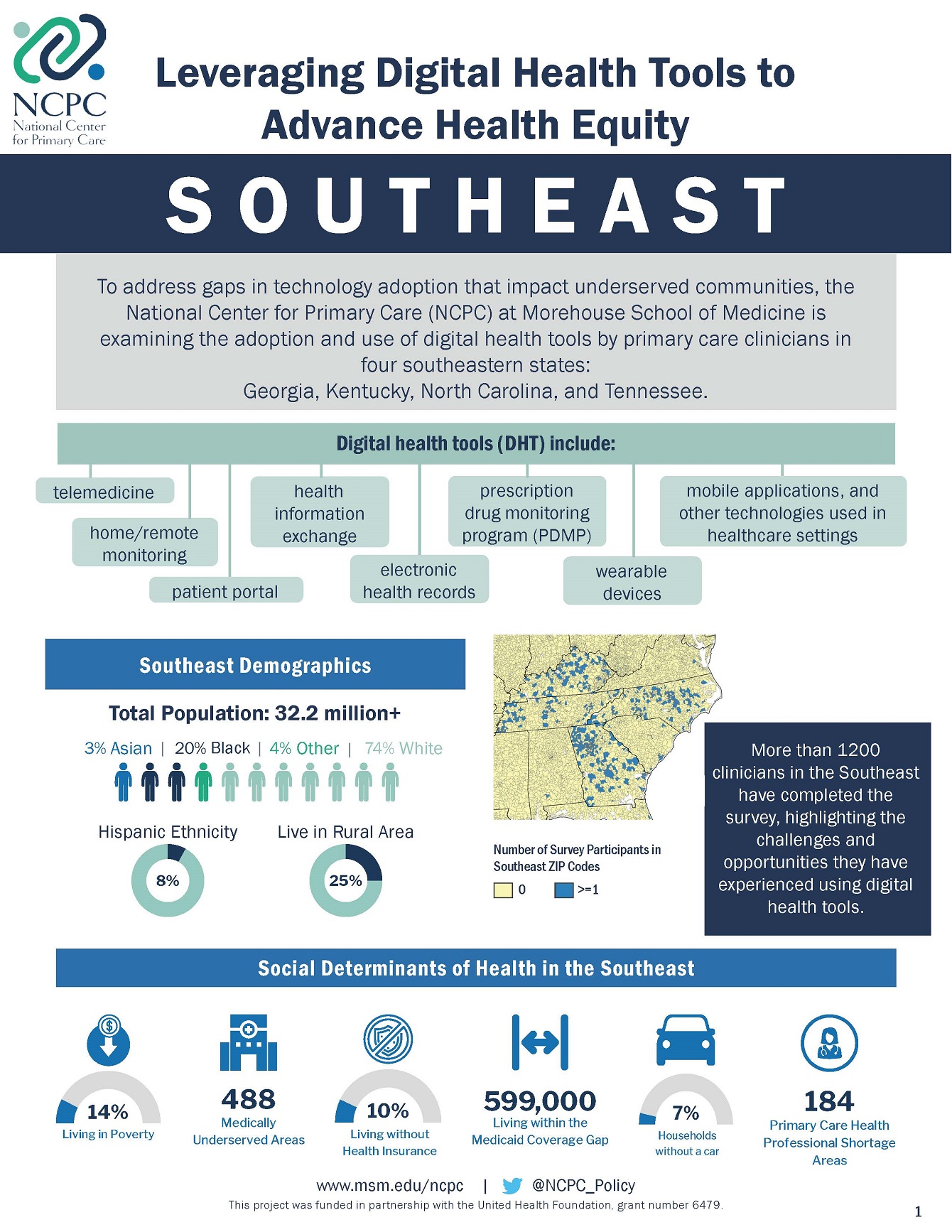
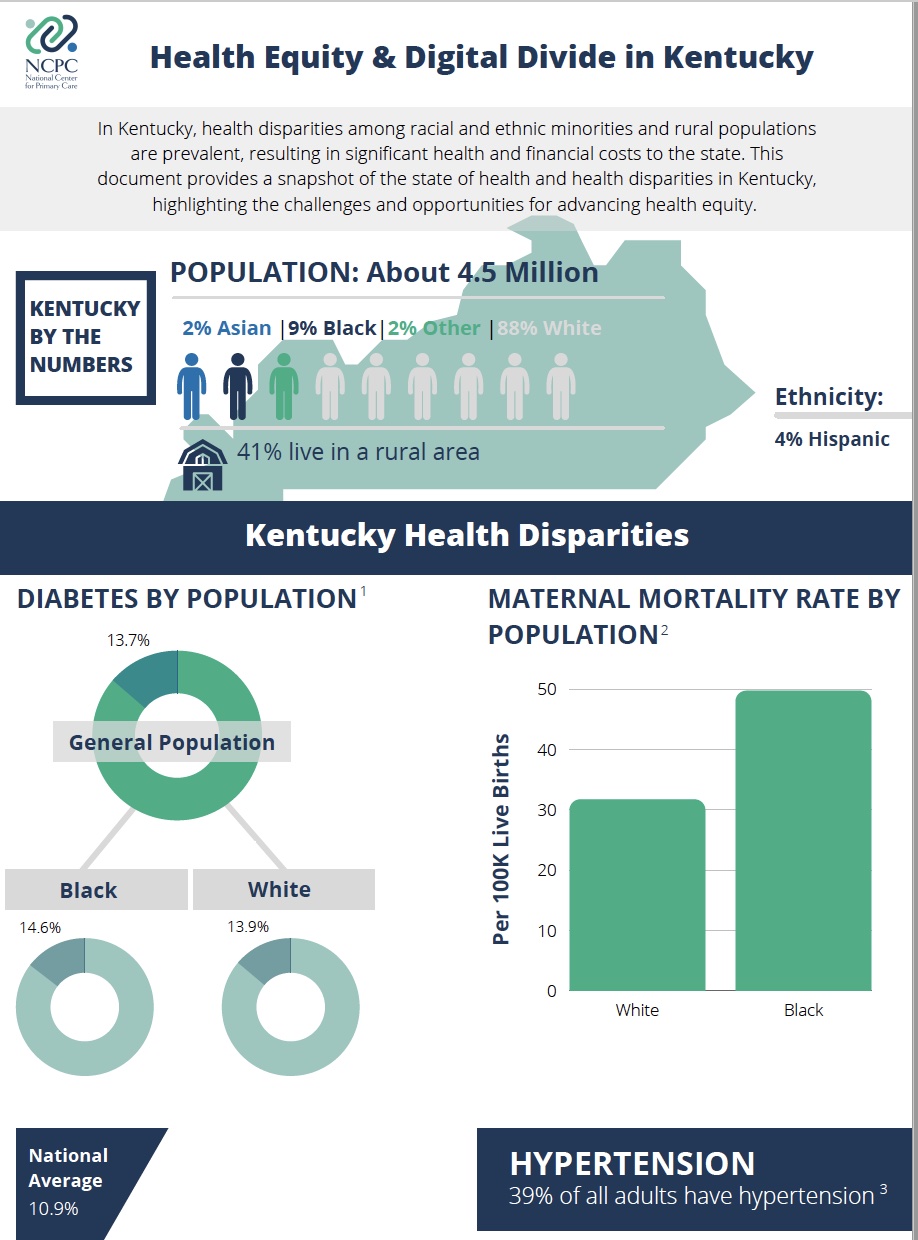
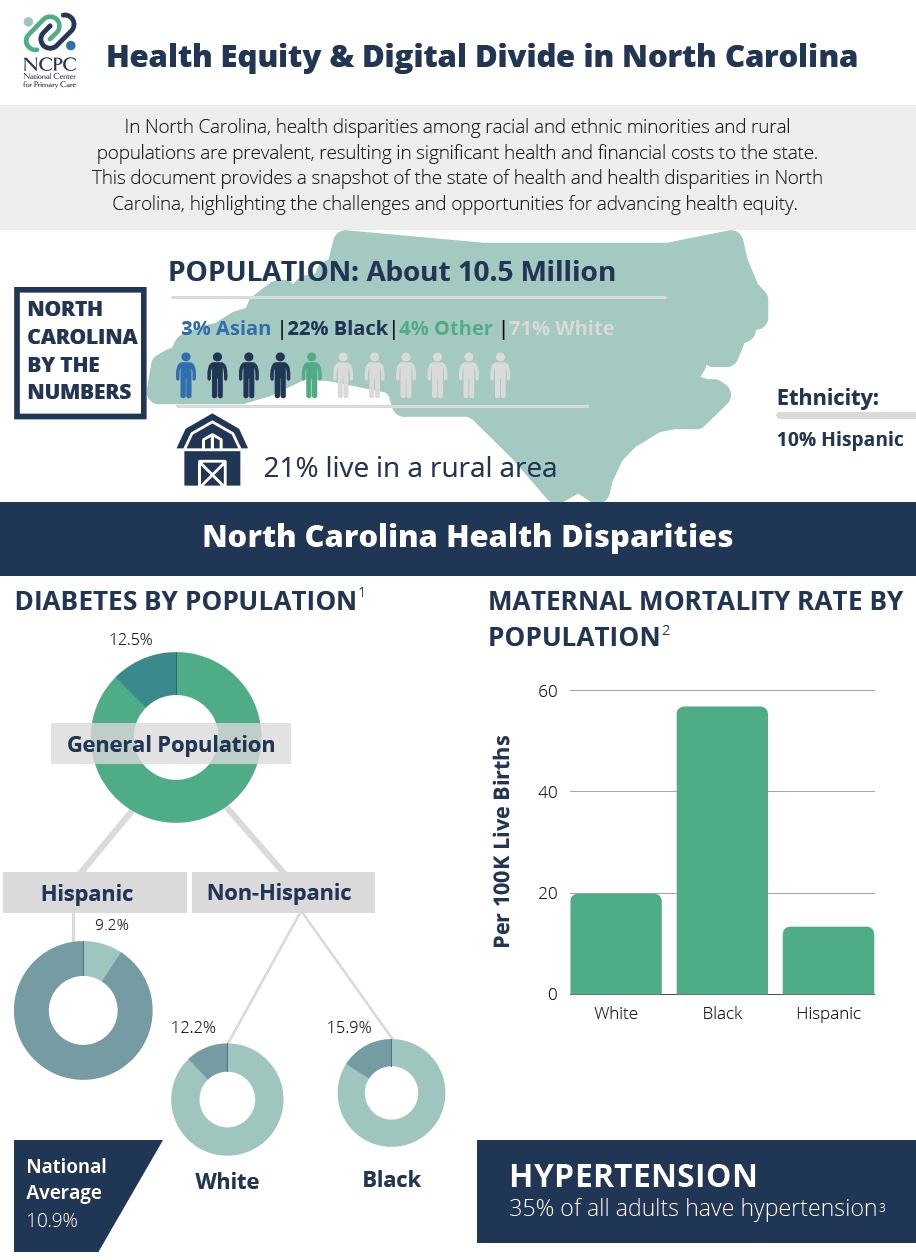
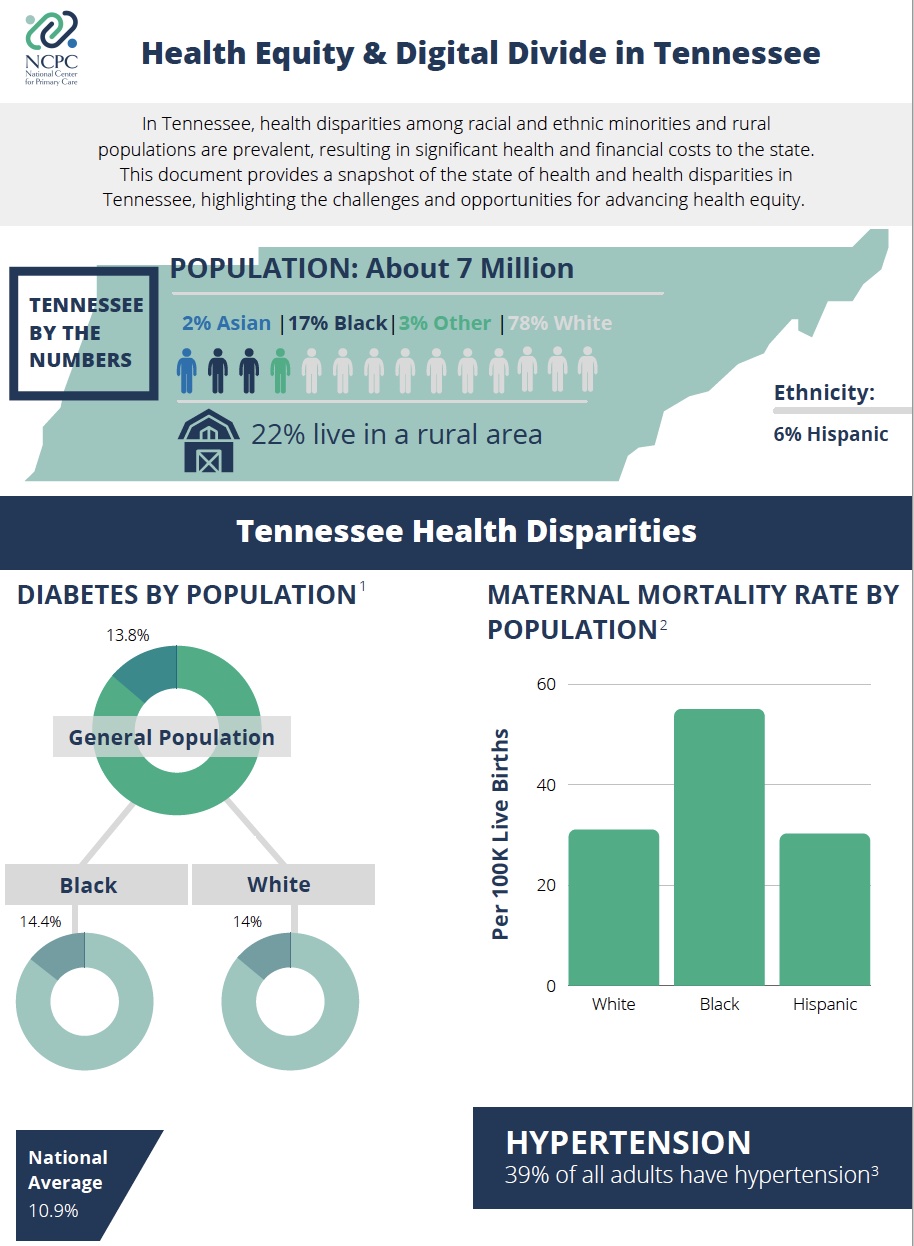
To address these gaps, the National Center for Primary Care (NCPC) at Morehouse School of Medicine is examining the adoption and use of digital health tools by primary care clinicians (Family Medicine, General Internal Medicine, General Practice, Pediatrics, or OB/GYN specialized physicians, nurse practitioners, physician assistants, and certified nurse midwives) in four southeastern states: Georgia, Kentucky, North Carolina and Tennessee.
We are prioritizing clinicians serving underserved communities in the southeast region due to the prevalent health disparities and poor health outcomes experienced by residents of these communities, with a particular focus on diabetes and maternal morbidity and mortality.
Our research strategy consists of the NCPC Digital Health Tool survey and focus groups of primary care clinicians working in the states of interest. We will also be conducting key informant interviews with policymakers, leadership, administrators, and staff in small practices and rural hospitals and conducting an environmental scan of the policy and system-level factors in each state to identify the facilitators and barriers to utilization of digital health tools in practice.
DIGITAL HEALTH TOOLS STUDY FINDINGS
Abstracts
Presentations
Reports
 |
 |
 |
 |
Publications
|
|
 |
 |
 |
Leadership Roundtable Briefs
|
|
|
|
This program is funded in partnership with the United Health Foundation.![]()
1Mack D, Zhang S, Douglas M, Sow C, Strothers H, Rust G. Disparities in Primary Care EHR Adoption Rates. J Health Care Poor Underserved. 2016 Feb;27(1):327-338.
Douglas MD, Xu J, Heggs A, Wrenn G, Mack DH, Rust G. Assessing Telemedicine Utilization by Using Medicaid Claims Data. Psychiatr Serv. 2017 Feb 1;68(2):173-178.
Douglas MD, Dawes DE, Holden KB, Mack D. Missed policy opportunities to advance health equity by recording demographic data in electronic health records. Am J Public Health. 2015 Jul;105 Suppl 3:S380-8.